
Understanding Your Hormones and Warning Signs
Hormones are the body’s chemical messengers. They travel through the bloodstream, coordinating everything from metabolism and mood to fertility and bone health. For women, two hormones play particularly significant roles: estrogen and progesterone. These work together in a delicate balance, influencing the menstrual cycle, pregnancy, and long-term well-being.
When this balance is disrupted, the effects can be drastic. Some women experience subtle changes they dismiss as stress or ageing. Others face symptoms significant enough to affect their daily lives. Recognising the warning signs early can make all the difference in protecting your health.
What Is Estrogen?
Estrogen is one of the primary sex hormones in the female body. The ovaries produce most of it during reproductive years, though the adrenal glands and fat tissue also contribute smaller amounts. After menopause, estrogen production declines significantly as the ovaries cease their reproductive function.
This hormone does far more than regulate menstruation. Estrogen affects multiple body systems:
- Reproductive system: Regulates menstrual cycles, supports ovulation, and maintains vaginal health
- Cardiovascular system: Helps maintain healthy cholesterol levels and reduces blood vessel inflammation
- Skeletal system: Supports calcium absorption and maintains bone density
- Brain and nervous system: Influences mood, memory, and cognitive function
- Skin and hair: Maintains collagen production and skin elasticity
- Urinary system: Supports bladder and urethral tissue health
What Is Progesterone?
Progesterone is the second major sex hormone in women, working alongside estrogen to regulate reproductive health. The corpus luteum — a temporary gland that forms after ovulation — produces most progesterone during the second half of the menstrual cycle. During pregnancy, the placenta takes over progesterone production after approximately ten weeks.
Key functions of progesterone include:
- Uterine preparation: Stabilises and maintains the uterine lining for potential implantation
- Pregnancy support: Sustains early pregnancy until the placenta takes over hormone production
- Cervical mucus: Thickens mucus after ovulation, creating a barrier to sperm and infections
- Breast tissue: Prepares mammary glands for potential milk production
- Mood regulation: Influences neurotransmitters that affect sleep, anxiety, and overall wellbeing
- Bone health: Works with estrogen to support bone mineral density
The Estrogen-Progesterone Balance
These two hormones function as a coordinated pair. When their levels are balanced, menstrual cycles remain regular, mood stays stable, and the body functions optimally. Problems arise when this balance tips too far in either direction.
Estrogen dominance occurs when estrogen levels are elevated relative to progesterone. This can happen when the body produces too much estrogen, metabolises it differently, or when progesterone levels fall too low.
Signs of estrogen dominance may include:
- Heavy or prolonged menstrual bleeding
- Breast tenderness or fibrocystic changes
- Mood swings, irritability, or anxiety
- Weight gain, particularly around hips and thighs
- Bloating and water retention
- Headaches or migraines, especially premenstrually
Hormonal Changes Throughout the Menstrual Cycle
Understanding how hormones rise and fall during a typical menstrual cycle helps explain many symptoms women experience. A complete cycle typically lasts 21 to 35 days, with 28 days considered average. Four key hormones orchestrate this monthly process: follicle-stimulating hormone (FSH), luteinising hormone (LH), estrogen, and progesterone.
Phase-by-Phase Breakdown
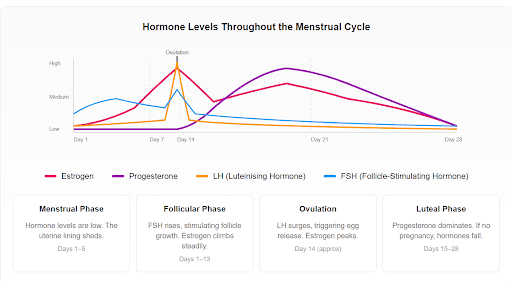
Menstrual Phase (Days 1–5): The cycle begins on the first day of menstrual bleeding. At this point, both estrogen and progesterone are at their lowest levels. The uterine lining, no longer supported by progesterone, sheds through menstruation. Many women experience fatigue and lower energy during this time.
Follicular Phase (Days 1–13): Overlapping with menstruation, the pituitary gland releases FSH, which stimulates the ovaries to develop follicles containing immature eggs. As follicles mature, they produce increasing amounts of estrogen. Rising estrogen thickens the uterine lining and often brings improved energy, mood, and mental clarity.
Ovulation (Around Day 14): The sharp rise in estrogen triggers a surge of LH from the pituitary gland. This LH surge causes the dominant follicle to release a mature egg. This is the most fertile window of the cycle. Some women notice mild pelvic discomfort, increased cervical mucus, or heightened libido around ovulation.
Luteal Phase (Days 15–28): After releasing the egg, the empty follicle transforms into the corpus luteum and begins producing progesterone. This hormone stabilises the uterine lining in preparation for potential implantation. If pregnancy does not occur, the corpus luteum breaks down, progesterone and estrogen levels fall, and menstruation begins again.
Warning Signs of Hormonal Imbalance
Hormonal imbalances can manifest in different ways, depending on which hormones are affected. Some symptoms are subtle and easy to dismiss, while others can significantly impact daily life. If you’re experiencing any of the following, it may be worth speaking with a healthcare provider.
| Menstrual Symptoms | Physical Symptoms | Mood & Cognitive Symptoms | Reproductive Symptoms |
| Irregular cycle length (shorter than 21 or longer than 35 days) | Unexplained weight gain or loss | Anxiety or depression | Difficulty conceiving |
| Absent periods for 3+ months | Persistent fatigue despite adequate rest | Mood swings beyond normal PMS | Recurrent pregnancy loss |
| Unusually heavy or prolonged bleeding | Hot flushes or night sweats | Difficulty concentrating (“brain fog”) | Vaginal dryness |
| Severe menstrual cramps | Skin changes, acne, or dryness | Memory problems | Reduced libido |
| Spotting between periods | Hair thinning or excess body hair | Sleep disturbances or insomnia | Pain during intercourse |
Conditions Associated with Hormonal Imbalance
Several medical conditions either cause or result from hormonal disruption. Understanding these connections helps explain why early detection and treatment matter.
Polycystic Ovary Syndrome
PCOS is the most common hormonal disorder affecting women of reproductive age, with an estimated prevalence of 10 to 18% globally. Elevated androgen levels, irregular or absent ovulation, and polycystic ovarian morphology characterise the condition.
Beyond reproductive symptoms, PCOS carries significant metabolic implications. Insulin resistance affects 65 to 95% of women with the condition, increasing the risk of type 2 diabetes. Women with PCOS who are overweight face higher rates of hypertension, high cholesterol, and cardiovascular disease. The hormonal imbalance also increases the risk of endometrial cancer due to prolonged exposure to estrogen without adequate progesterone.
A fertility specialist can help assess overall risk and recommend appropriate monitoring. Regular screening for blood glucose, cholesterol, and blood pressure should be part of ongoing care for women with this condition.
Thyroid Disorders
The thyroid gland produces hormones that regulate metabolism, energy levels, and body temperature. Imbalances can significantly affect menstrual regularity and fertility.
| Condition | Cause | Common Symptoms |
| Hyperthyroidism(Overactive thyroid) | Excess thyroid hormone production | Rapid heartbeat, weight loss, anxiety, heat intolerance, tremors, light or absent periods |
| Hypothyroidism(Underactive thyroid) | Insufficient thyroid hormone production | Fatigue, weight gain, cold sensitivity, depression, heavy or irregular periods, constipation |
Untreated hypothyroidism during pregnancy increases the risk of complications and may affect fetal development. Hashimoto’s thyroiditis, an autoimmune condition that attacks the thyroid, is more common in women and often occurs alongside other hormonal imbalances.
Consequences of Untreated Hormonal Imbalance
The body’s systems are interconnected, and prolonged hormonal disruption can set the stage for chronic health conditions.
Long-term health risks of untreated hormonal imbalance:
- Cardiovascular disease: Increased risk of heart disease, hypertension, and stroke, particularly with PCOS or post-menopause
- Osteoporosis: Accelerated bone loss leading to fractures, especially with low estrogen
- Type 2 diabetes: Progression from insulin resistance to impaired glucose tolerance and diabetes
- Infertility: Difficulty conceiving due to irregular ovulation or inadequate progesterone
- Endometrial cancer: Increased risk from prolonged estrogen exposure without progesterone
- Cognitive decline: Potential increased risk of memory problems and dementia
A Holistic Approach to Hormonal Health
Managing hormonal imbalance typically involves a combination of lifestyle modifications and, when necessary, medical treatment:
- Regular physical activity: At least 150 minutes of moderate exercise weekly improves insulin sensitivity, supports weight management, and helps regulate hormone levels
- Balanced nutrition: A diet rich in vegetables, fruits, whole grains, lean proteins, and healthy fats supports metabolic function; limiting refined carbohydrates and added sugars helps maintain stable blood glucose
- Quality sleep: Aim for seven to nine hours nightly, maintaining consistent sleep and wake times
- Stress management: Techniques such as mindfulness, breathing exercises, or regular physical activity help regulate cortisol levels
- Maintaining healthy weight: Even modest weight loss (5–10%) can significantly improve hormonal balance in overweight women with PCOS
When to Seek Medical Evaluation
Specific symptoms require a professional assessment. Consider scheduling an appointment if you experience:
- Persistent menstrual irregularities lasting more than three cycles
- Periods that suddenly become significantly heavier or more painful
- Absent periods for three months or more (if not pregnant)
- Unexplained weight changes of more than 5% of body weight
- Persistent fatigue that interferes with daily activities
- New onset of mood symptoms such as anxiety or depression
- Difficulty conceiving after 12 months of trying (or 6 months if over 35)
- Signs of hormonal conditions such as acne, excess facial hair, and irregular cycles
Medical Treatment Options
Various medical treatments can also be used to help restore hormonal balance:
- Combined oral contraceptive pills: Regulate menstrual cycles and reduce androgen levels in conditions like PCOS
- Progestogen therapy: Protects the uterine lining in women with irregular cycles
- Menopausal hormone therapy: Relieves symptoms such as hot flushes, night sweats, and vaginal dryness
- Metformin: Manages insulin resistance in PCOS
- Thyroid medication: Restores normal thyroid hormone levels
- Ovulation induction: Prescribed under specialist supervision for women seeking pregnancy
The Malaysian Clinical Practice Guidelines on Management of Menopause recommend individualised treatment decisions based on symptom severity, medical history, and patient preferences. Therapy should use the lowest effective dose for the shortest necessary duration.
Key Takeaways
- Estrogen and progesterone work together to regulate menstrual cycles, fertility, and long-term health including cardiovascular and bone health.
- Hormone levels rise and fall predictably during the menstrual cycle — understanding these patterns helps identify when something is wrong.
- Warning signs of hormonal imbalance include irregular periods, unexplained weight changes, persistent fatigue, mood disturbances, skin changes, and difficulty conceiving.
- PCOS affects 10 to 18% of women and carries increased risks of type 2 diabetes, cardiovascular disease, and endometrial cancer if left unmanaged.
- Untreated hormonal imbalance can lead to serious long-term consequences including osteoporosis, heart disease, metabolic disorders, and fertility problems.
- Lifestyle modifications — including regular exercise, balanced nutrition, adequate sleep, and stress management — form the foundation of hormonal health.
- Regular health screening enables early detection of hormonal and metabolic problems, allowing for timely intervention.
Understanding your hormones is the first step toward taking control of your health. If you have noticed changes in your menstrual cycle, unexplained symptoms, or have concerns about your hormonal health, our team at SpringHill Clinic is here to help. We provide comprehensive assessments and personalised care in a supportive, confidential environment. Book an appointment today.
